Abstract
Background
The incidences of Aplastic anemia (AA) vary, reportedly being lower in North America and Europe, and three to five times higher in Asia.
Definitive therapy for AA include hematopoietic stem cell transplantation (HSCT) and immunosuppressive therapy (IST).
In patients whose age > 40 and without HLA-MSD, IST with horse anti-thymocyte globulin (h-ATG) and cyclosporine are still the first choice but h-ATG is not available in some Asia, including Taiwan. Hence, allogeneic HSCT for Asian SAA patients might be of more importance.
The use of peripheral blood stem cell transplantation (PBSCT) has increased in recent years in the majority of centers, but bone marrow (BM) was the preferable graft source in recipients in previous studies, so there are insufficient data to support the use of PBSCT.
We conducted a cohort study to report the outcomes of SAA patients receiving allogeneic HSCT.
Methods
SAA patients receiving allogeneic HSCT consecutively between 1985 and 2015 were enrolled. All patients were followed up until death, and the date of latest follow-up, or April 31, 2016. The maximum follow-up period was 31 years. Patients receiving cord blood stem cell transplant were excluded because of a large proportion of graft failures reported.
Rather than the standard conditioning regimen: Cyclophosphamide 200mg/kg (CY-200) and ATG, we used CY-200 and total body irradiation (TBI) (range 200-1,200 cGy). Rabbit ATG (r-ATG) was added additionally in the conditioning regimen for 59 (39.6%) patients at physicians' discretion.
We used chi-square tests or Fisher's exact test to compare the categorical variables between the two groups. Data are presented as medians and interquartile ranges (IQR) for skewed data. The cutoff value of time to HSCT (i.e., three months) and transplant year (year 2000) was chosen according to the median.
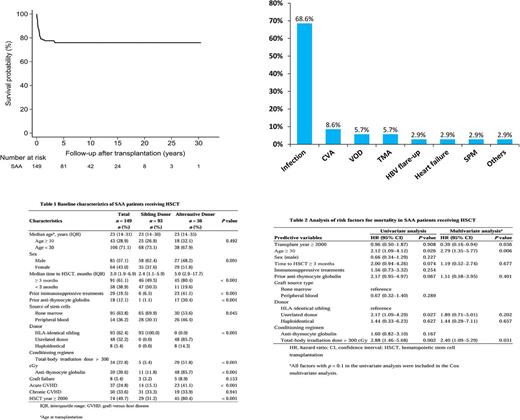
The primary endpoint was mortality. The survival probability was estimated using the Kaplan-Meier method. The risk factors for mortality were calculated using a Cox proportional hazards model, and hazard ratios (HRs) and the 95% confidence intervals (CIs) were calculated. We used a multivariate Cox proportional hazards model to identify risk factors for mortality while adjusting for possible independent confounding factors. All risk factors with p < 0.1 in the univariate model were entered into the multivariate analysis. All statistically significant levels were set at p < 0.05.
Results
A total of 151 SAA patients were identified. Two patients receiving cord blood transplantation were excluded.
The median age at transplant was 24 (IQR 14-31 years), and 64 (43.0%) were male. The median time to HSCT was three months (IQR 1.9-6.9 months).
The Clinical characteristics of the cohort are shown in Table 1. The patients receiving HSCT from unrelated donors versus sibling donors, more receiving peripheral blood stem cell than bone marrow as graft source in unrelated donors
The overall survival rate (OS) was 76.0% within 31 years of follow-up (Figure 1).
Eight patients (5.4%) failed engraftment, including seven primary graft failures and one secondary graft failure after seven years of transplantation. Two of them received second allogeneic HSCT and survived. Incidences of acute and chronic GVHD were 24.8% and 33.6%, respectively.
The causes of mortality are shown in Figure 2. Infection was the leading cause of mortality
The analysis of the risk factors of mortality is detailed in Table 2.
Seven patients (4.7%) developed posttransplant malignancies, including four cases of posttransplant lymphoproliferative disease (PTLD), two cases of head and neck squamous cell carcinoma (SCC) and one case of esophageal SCC. Only one patient of PTLD died.
Conclusion
In the lack of h-ATG, we adopted CY 200-TBI as the conditioning regimen rather than the standard CY 200-ATG and reported OS of 76.0% in 149 SAA patients receiving allogeneic HSCT in Taiwan. Infection is still the major mortality cause and should be monitored cautiously.
Despite TBI as a concern for developing malignancies, only one patient in our cohort died of PTLD.
We have identified the age at transplantation of ≥ 30, conditioning regimen with TBI > 300 cGy, and transplant year < 2000 were independent predictors of death, indicating the outcomes improved chronologically.
The comparison between PBSC and BMSC remained an unresolved issue so far. Herein, PBSCT is not a risk factor for death versus BMT in our cohort.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal